Pain Stories: Dr. Frank H Gawin, Pain and Forced Opioid Tapering
“a constant battle between myself and my physician.”
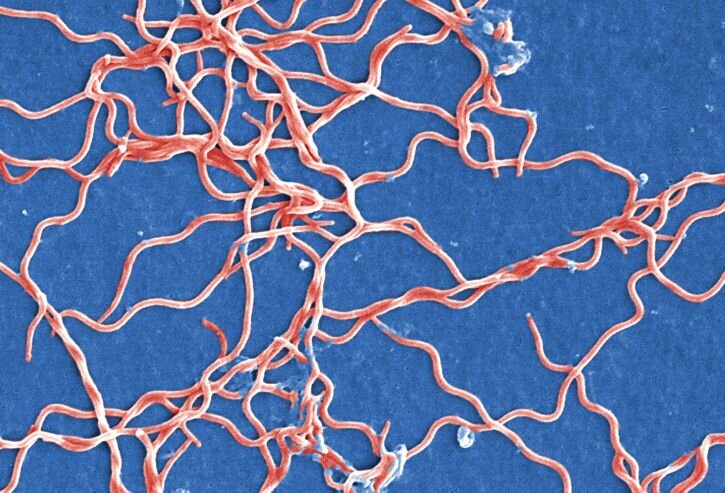
Addiction medicine specialist, Dr. Frank Gawin, was two years into his work at Yale University, as the Scientific Director of Stimulant Abuse Research, when his trek through a Connecticut salt marsh yielded a tell-tale sign: the distinctive “bulls eye” rash from a Lyme infected tick bite. Soon after noticing the rash, Dr. Gawin developed other symptoms of Lyme disease—swelling, high fever, muscle pain, infections, fatigue and cognitive fog.
His family struggled to adjust to his diminished capacity.
Despite having access to the best available care, his symptoms only worsened. Dr. Gawin tried more than 40 medications—from antidepressants to antibiotics, and mast cell inhibitors to allergy treatments—to address his debilitating joint pain, extreme weakness and waning concentration. At work, he struggled on, continuing to receive National Institute on Drug Abuse grants and to publish important scientific articles. But there were other costs. His family struggled to adjust to his diminished capacity. He and his then-wife ultimately divorced.
By 1990, four years after he was first diagnosed, Dr. Gawin’s disease had progressed to its most severe form: he developed Neuro-Borreliosis, a condition of the central nervous system that occurs in 2-4% of Lyme cases. With this disease progression, Dr. Gawin suffered a cascade of additional symptoms. He developed severe asthma, often falling into short-term comas. His neuropathic pain—the pain caused by the disease and damage in his central nervous system—grew intractable and increasingly severe. The compounding conditions intensified as the years drew on.
Dr. Gawin describes his pain as feeling as if someone were stabbing him repeatedly with a knife. The pain never remits; its intensity varies, but the knife—the stabbing sensation—is ever-present. He also has a grinding pressure in his hips and knees, and the eerie sensation of crawling beneath his skin.
“as if someone were stabbing him repeatedly with a knife…the eerie sensation of crawling beneath his skin. ”
In 1994, Dr Gawin was first prescribed opioids to manage his pain. With this medication, his joint pain and the neurological symptoms that most threatened his ability to work came under better control. He was able to approach his career with renewed vigor, and even to reach previous levels of rigorous academic research and publication. Altogether, Dr. Gawin has authored approximately 100 scientific articles and his work has been featured on ABC, CBS, NBC, and CNN, as well as in Newsweek, The New York Times, Washington Post, The Reader’s Digest and Scientific American. Dr. Gawin believes that pain management with opioids extended his ability to work by more than a decade.
Eventually, in 2007, Dr. Gawin retired due to increasing fatigue, fog, and pain from his disabling condition. He no longer has the quality of life he used to enjoy: he cannot mow the lawn, grocery shop, or do household chores. Social activities are interrupted by his need to rest after only an hour of sitting and visiting. He finds the isolation of pain to be the biggest challenge in his life.
The biggest challenge, that is, until 2016, when Dr. Gawin’s treating physician abruptly informed him during a routine visit that she would no longer prescribe his opioid regimen. Like many clinicians, Dr. Gawin’s doctor worried about running afoul of medical and legal authorities, after the Centers for Disease Control and Prevention (CDC) issued its Guideline for Prescribing Opioids for Chronic Pain which contained dosage recommendations. Due to increased oversight from the Drug Enforcement Agency and state medical board, she felt pressure to get him under the CDC’s recommended threshold of 90 morphine milligram equivalents. At that point, Dr. Gawin had been on the same dose of opioids with one minor adjustment for 15 years.
As his dosage was reduced by 10% each month, Dr. Gawin’s pain soared.
As his dosage was reduced by 10% each month, Dr. Gawin’s pain soared. He felt helpless and hopeless at the loss of the little quality of life he had. He wasn’t himself. He repeatedly asked for the evidence that would support the decision to taper him. It was, as he puts it, “a constant battle between myself and my physician.” Dr. Gawin suffered profoundly; he was diagnosed with Post Traumatic Stress Disorder (PTSD) related to the tapering experience.
Fortunately, after a lot of searching, Dr. Gawin found a physician who is willing to prescribe for him. But it requires that he travel from Hawaii where he and his current wife reside to the US mainland. The travel is expensive, painful and physically debilitating. And Dr. Gawin lives in constant fear that, at any moment, he will lose access to his treatment once again.